Diagnostics
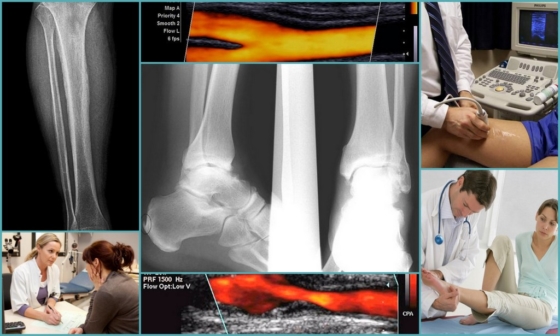
Post-thrombotic disease of the lower extremities is detected on the basis of an external examination by a doctor, using instrumental examination methods and anamnesis data. In the latter case, the patient is interviewed and the history of the previous illness is studied - if the patient was treated for thrombosis, the likelihood of PTFS is very high.
With the help of duplex scanning, the state of the venous wall, the speed of blood flow, the evacuation of blood and its outflow from the extremities are revealed. Also, ultrasound, passing through hard and soft tissues, provides information about the presence or absence of blood clots.
As an addition to the diagnosis of PTFS, an x-ray with the use of a contrast agent may be prescribed to the patient. After confirming the disease, appropriate treatment is prescribed.
Etiology and pathogenesis
Post-thrombotic disease develops after a thrombosis, since the veins can no longer fully recover and there are irreversible consequences that provoke the development of pathology. As a result, the vessel is deformed, the venous valves are damaged - their function is reduced or completely lost.
The main reasons for the development of PTFS cannot be described point by point, since one persistent violation leads to the formation of post-thrombophlebitic syndrome - thrombosis of a venous vessel. This disease leads to blockage of the lumen of the vein and impaired blood flow. Against the background of the treatment, after a few days, the thrombus begins to gradually dissolve, and the damaged vessel is filled with blood again.
But at this stage, there is one feature - after restoration, the vein is no longer able to fully perform its functions - it is deformed, its walls are not so smooth, and the valvular apparatus does not function well. All this leads to congestion and the development of insufficient pressure in the venous system of the extremities. Blood is not discharged through the perforating veins from deep vessels to superficial ones - therefore, post-thrombophlebitic syndrome captures all vessels of the lower limb.
Over time, there is an expansion of the subcutaneous and internal veins, a compression drop in pressure, a slowdown in blood flow and the appearance of new clots. As a result, the disease acquires a chronic course, there are constant signs and symptoms that disturb the patient.
Thrombosis and thrombolysis
This process can be divided into several stages:
- a thrombus is formed on the damaged vascular wall to prevent blood loss, partially or completely blocking the lumen of the vessel (the size of the clot depends on the nature of the damage);
- partially or completely blocked blood flow reduces the load on the vessel and makes it possible to fully restore damaged tissues;
- after healing of the damaged area, the thrombolysis mechanism is triggered, which is necessary to restore vascular patency;
- under the action of blood-thinning enzymes, the blood clot dissolves and normal blood flow is restored.
These mechanisms are typical for a healthy person when they receive an injury, but sometimes this is also possible in the initial stages of thrombosis. Natural thrombolysis in thrombosis can occur with a change in diet (inclusion in the menu of products that promote blood thinning), but only if the formation has a loose blood structure.
But in most patients, the formations that narrow the vascular lumen consist not only of platelets, atherosclerotic deposits are additionally attached to them and fibrinous threads are deposited on them. The body can no longer destroy such a dense structure on its own, and medications are used for this.
Surgical recanalization
The following types of surgical recanalization are performed:
- Thrombus removal is performed minimally invasively, endovascular therapy methods are used. Under local anesthesia, an incision is made, a catheter is inserted into the damaged vessel and, under the supervision of the operating physician, is brought to the site of the thrombus. Next, the clot is captured and removed from the vein.
- Bypass is used when the clot cannot be removed. A bypass path of blood flow is formed. The material is their own vessels - veins taken for plastic surgery, or synthetic analogues.
- Ligation involves the imposition of a ligature above and below the site of the clot, the blood flow is redistributed through small arteries and veins.
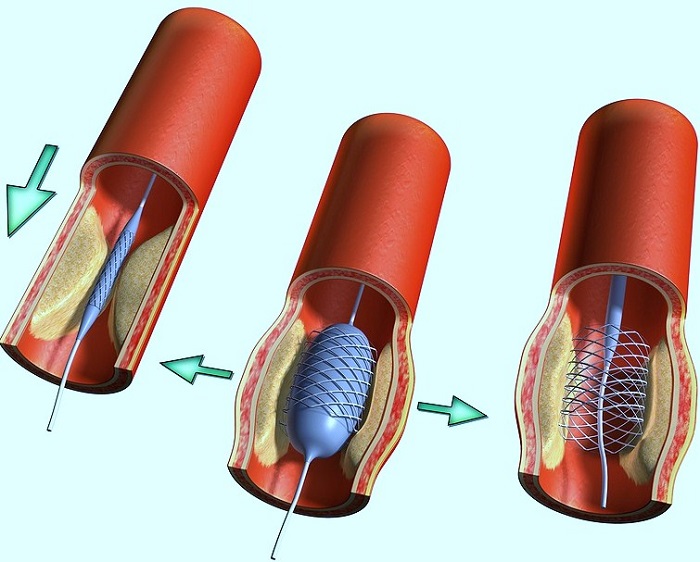
- Stenting is the insertion of a balloon that expands the vessel. Blood circulation improves and platelet aggregation on the affected wall decreases, but such an operation is advisable only with gradual thrombus formation.
Not always the operation is performed to restore blood flow. Recanalization of the umbilical vein is performed to provide access to the liver and gallbladder in case of their pathology. Infusion solutions are introduced through the catheter; in case of purulent damage to organs, antibacterial agents are delivered to the focus.
Thrombus recanalization is often a lengthy process that requires the attention of not only doctors, but also patients. To achieve the best result, as well as to prevent further thrombosis, the patient should reconsider the lifestyle, diet and consult a doctor in a timely manner at the first symptoms of the disease. Achievements of modern medicine can significantly increase the likelihood of a full recovery.
Vitamins and nutrition to strengthen the walls of blood vessels
Have you struggled with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day…
In addition, it is useful to eat cereals from various cereals - oatmeal, buckwheat, corn and rice. It would be better to replace pasta with cereals.
How to strengthen the walls of blood vessels? For this, it is also useful to eat legumes such as peas, beans, lentils, soybeans. Soy is just an indispensable product for healthy walls, since it contains all the minerals and compounds required by the body that help remove cholesterol from the body.
There are also vitamins to strengthen the walls of blood vessels. Vitamin P is very significant, which is extremely effectively absorbed by the body in combination with vitamin C. Vitamin 3 reduces fragility and restores elasticity to the walls. It is for this reason that foods that are rich in this compound of vitamins must be present in the daily diet.
Particularly invaluable plant products in strengthening the walls of blood vessels are onions, garlic and eggplant. They relieve the vessels of excess fat deposits and free the walls from fragility. Still effective are the active substances that are present in the composition of cucumbers.
As for fruits, grapefruit is the leader among citrus fruits, among berries it is worth noting red and black currants, as well as chokeberry. If it is impossible to eat fresh fruits and vegetables, it is better to include green tea, decoctions of chokeberry and rose hips in your diet.
In order to strengthen, it is recommended to harden with a contrast douche. The temperature difference and water pressure on the walls of the vessel trains the cardiovascular system well and develops a normal response to climatic, seasonal and weather changes. In addition, water procedures have a positive effect on the nervous system. There are also drugs that strengthen the walls of blood vessels.
See the continuation of this article here: strengthening of blood vessels part 2
Recanalization of the fallopian tubes and umbilical vein
Recanalization of the fallopian tubes is the restoration of their patency by removing connective tissue adhesions in their lumen.
This is a mechanical obstacle that often causes female infertility.
The process is asymptomatic, develops after infectious processes, abortions, long-term use of spirals.
Such manipulation can be carried out on an outpatient basis. A catheter is inserted and, under the control of cameras, adhesions are dissected.
Through the restored umbilical vein, it is possible to administer infusion solutions for a long time during operations on the liver and biliary tract.
In purulent diseases, abscesses, antibiotic solutions are administered.
The technique is contraindicated in local inflammatory processes, kidney tumors that compress the portal vein.
Definition of vein recanalization options for solving the problem
At the first contact with a specialist, and a proposal to conduct recanalization, patients are frightened because of a lack of understanding of what they will be doing. You need to know that vein recanalization after thrombosis is the restoration of vascular patency, which can be achieved in various ways. There are 3 main methods for restoring venous patency:
- Independent, or natural.
- Conservative, or medicinal.
- Operative, or surgical.
Under normal conditions, the formation of a blood clot is a protective reaction of the body, which is aimed at preventing the development of bleeding.
Under certain conditions: blood clotting, increased activity of the coagulation system, hereditary predisposition, impaired venous outflow, this process becomes pathological.
The resulting thrombus can partially or completely block the lumen of the vessel, when it is torn off, an embolism develops, from which you can die. If the thrombus is overgrown with connective tissue, then it will not resolve on its own.
With a balanced work of the blood coagulation system, immediately after the formation of a blood clot, the fibrinolytic system is launched. Its activity is aimed at the disorganization and resorption of a blood clot due to special substances. Such a variant of the destruction of a thrombus is possible at the initial stages, while it has a loose structure.
Medical recanalization is carried out in the absence of a threat of a blood clot or partial blockage of the vessel, which cannot lead to the loss of the function of a vital organ. There are several groups of drugs used alone or in combinations.
The list of groups, the main representatives and the effect they have are presented in the table.
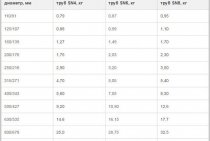
| Drug group | Name | Action taken |
| Anticoagulants of direct and indirect action | unfractionated heparin, low molecular weight heparin, warfarin | They have little effect on the resorption of an existing thrombus, but prevent its growth and increase in diameter and length. |
| Antiplatelet agents | Aspirin, Curantyl | They inhibit the process of platelet aggregation, that is, gluing them together |
| fibrinolytic agents | Streptokinase, Alteplase | Dissolve thrombus quickly |
| Angioprotectors | Detralex, Venarus | They do not take part in the resorption of a blood clot, but inhibit thrombus formation |
In situations where there is no serious danger to life, direct-acting anticoagulants, heparins, are more often used.
The duration of therapy with them reaches a year or more. Additionally, antispasmodics, antioxidants, drugs that improve blood rheology are prescribed.
What is operative vein recanalization? Surgical methods are used in cases where it is necessary to quickly eliminate the problem, with complete occlusion of the vessel, a high risk of thrombus separation and embolism. Several methods are used:
- thrombectomy - removal of a blood clot from the lumen of the vessel.In 1946, the first successful operation of this type was performed, and today they are performed in all major surgical centers in the world;
- shunting - creating bypass routes;
- stenting - the installation of a special stent (a device that expands the lumen of the vessel), which restores the normal movement of blood.
The selection of the method of surgical treatment is carried out by a vascular surgeon based on the results of additional research methods. The location of the thrombus, its prevalence, the state of other vessels are taken into account.
Recanalization of veins. What is classification.
Recanalization is the process of restoring the patency of a vessel whose lumen is closed by a thrombus. Vein recanalization occurs in one of three ways:
- natural;
- medical;
- surgical.
Natural recanalization is a physiological process. It occurs under the influence of aseptic fibrinolysis. The clot is eliminated independently in almost half of the cases. In addition to the destruction of a thrombus, its revascularization is possible: it grows into microvessels, collagen structures. There is a restoration of the patency of the vessel and acceleration of the destruction of the clot. Self-elimination of blockage is possible at the stage of a “loose” thrombus. When it is overgrown with connective tissue, fibrinolysis is difficult.
However, sometimes the body cannot cope with the dissolution of a blood clot: blood clotting, increased clotting activity, genetic predisposition, impaired venous circulation make this process difficult. The resulting clot blocks the lumen of the vessel, can cause an embolism - a life-threatening condition. In these cases, medical recanalization is indicated.
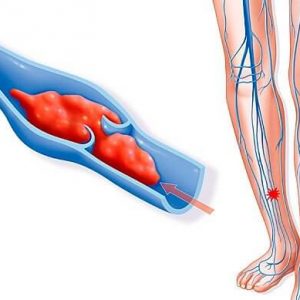
Deep vein thrombosis of the lower extremities
The deep venous system of the lower extremities plays a major role in the outflow of venous blood from the lower extremities, normally providing an outflow of 80-90% of the blood.
When deep vein thrombosis occurs in the lower extremities, the outflow of most of the blood from the lower extremities becomes difficult. Deep vein thrombosis is a condition that occurs as a result of the formation of a blood clot in the lumen of the veins of the lower extremities.
This condition is life-threatening, due to the possibility of a thrombus detachment and its migration with the blood flow to the pulmonary artery, which in this case leads to the occurrence of pulmonary embolism.
Deep vein thrombosis is one of the main causes of pulmonary embolism. In turn, approximately one third of all sudden deaths are caused by pulmonary embolism.
Causes of deep vein thrombosis
Various causes lead to the occurrence of deep vein thrombosis, including trauma to the extremities, recent surgical interventions, oncological diseases, chemotherapy treatment, prolonged immobilization and physical inactivity, hematological diseases, superficial varicothrombophlebitis, hormonal contraceptives, pregnancy and the postpartum period, obesity, old age and etc.
Symptoms of thrombosis
The clinical picture is directly proportional to the degree of spread of the thrombotic process. In the initial stage of thrombus formation, pain in the lower limb, swelling, and fever occur.
In cases of total thrombosis of the deep system with the transition to the iliac veins, blue phlegmasia may develop, which characterizes a violation of the general condition, high temperature, a change in the color of the skin to a purple hue, an increase in the circumference of the limb several times and a pronounced pain syndrome.
There are several stages of the thrombotic process: the stage of thrombus formation, the stage of organization and the stage of recanalization. Thrombosis is most dangerous in the initial stage, when thrombotic masses are not yet fixed to the vein wall. During this period, the highest probability of thromboembolism.
Subsequently, the thrombus is organized and fixed to the wall of the vein. In certain cases, a floating thrombus occurs - a freely “dangling”, not fixed top of a thrombus, which poses a threat of separation.
After the expiration of time, the thrombus recanalization occurs - the resorption of the thrombus with the restoration of the lumen of the vein to one degree or another. But, unfortunately, the valves that regulate the unidirectional blood flow irrevocably die, which leads to the development of post-thrombophlebitic syndrome.
Methods for the treatment of deep vein thrombosis
Methods of treatment depend on the stage of the disease, the state of thrombotic masses and the prevalence of the thrombotic process. Treatment is predominantly conservative, in some cases surgical treatment is indicated.
The earlier treatment is started, the more favorable the prognosis - the risk of thromboembolism decreases many times over, further spread of the thrombus stops, recanalization (recovery) of the vessel lumen occurs to a greater extent, and therefore the manifestations of post-thrombophlebitic syndrome are minimized for the rest of life.
https://www.youtube.com/watch?v=9R8tIqtxOPM
If there are complaints clinically and with the help of instrumental research methods, it is possible to make a correct diagnosis and prescribe a course of necessary treatment, and in some cases save the patient's life.
In ACMD-Medox you will be consulted by a vascular surgeon, if necessary, you will be carried out ultrasound diagnostics of blood vessels (duplex scanning of blood vessels) and other instrumental studies.
Remember! Early referral to a vascular surgeon contributes to more effective treatment and a better long-term prognosis.
Methods for diagnosing vascular damage
They resort to the use of laboratory and instrumental diagnostic methods. For laboratory analysis, venous blood is used, a coagulogram, or a hemostasiogram is examined. It reflects the activity of the coagulation and anticoagulation systems. Determine the level of fibrinogen, thrombin, prothrombin, prothrombin index and activated partial thromboplastin time (APTT). Each of these indicators is important and diagnostically valuable.
In routine practice, non-invasive, that is, not requiring integrity violations, methods of instrumental diagnostics are used. These are ultrasound of vessels with dopplerography, angiography of vessels with a contrast agent, if necessary, MRI with contrast.
Medical recanalization
If there is no life-threatening condition (the risk of a blood clot breaking off or a blockage of vital vessels that has already occurred), then conservative treatment is applied first. Depending on the site of thrombus formation, a drug is selected.
It can be:
Fibrinolytics. The drugs of this group (Alteplase, Streptokinase) are administered intravenously and contribute to the rapid destruction of thrombosis, but their use causes many adverse reactions. The need for rapid thrombolysis appears when vital arteries are blocked (heart attack or PE - pulmonary embolism).
- Angioprotectors. They almost do not participate in the process of lysis, but prevent further thrombosis. These include funds such as Detralex and Aescusan.
- Antiplatelet agents. Means that reduce the ability of platelets to aggregate (stick together). The most famous drug is Aspirin, which is used in cardiology to prevent thrombotic complications. And also this group includes Curantil, Thrombo-Ass, Tirofiban, etc. (the list of drugs is very large).
- Anticoagulants. Drugs that promote active blood thinning. The most famous representatives of this group are Warfarin and Heparin.
But if there is no life-threatening condition, the recanalization process is slow and takes about six months (sometimes more).Additionally, patients are prescribed vasodilator drugs and medications that improve blood flow.
In most cases, if the disease was detected in a timely manner, then the walls of the artery are completely cleared and restore their tone, and on the veins, the presence of the disease after successful treatment may be indicated by a slightly expanded and slightly deformed area.
Prognosis and complications
The prognosis for post-thrombophlebitic vein lesions is relatively favorable in cases where the patient adheres to the doctor's basic recommendations - does not violate the treatment program and follows the basic rules to prevent recurrence of the disease. With this approach, you can achieve a supportive optimal state for a long time.
If the rules of the wellness program are violated, the patient experiences complications in the form of circulatory disorders in the limbs, which can lead to gangrene requiring amputation. The second serious complication is heart attacks of the brain or internal organs when a blood clot enters the general bloodstream.
Treatment and symptoms of deep vein thrombophlebitis of the lower extremities
The formation of blood clots in the lumen of the veins is a fairly common phenomenon and is called acute deep vein thrombosis of the lower extremities. In this disease, 27–35% of patients develop arterial thromboembolism in the lungs.
Thrombophlebitis of the veins of the lower extremities occurs relatively rarely in healthy people, and the number of diseases increases every year.
Therefore, the development and application of conservative treatment of the disease is an important task in vascular surgery.
Thrombophlebitis of deep veins
Vein thrombi occur for various reasons and develop with a normal epithelial layer on the vessel wall. Their formation begins in the veins of the lower leg - on their valves, where blood clotting factors accumulate due to the vortex blood flow through the valve leaflets and in the area of venous division.
Platelets provoke early thrombosis by settling on the valves of the veins and at points with impaired integrity of the epithelial layer.
They attach to the endothelium, or to the exposed collagen layer on the walls of the veins. The subsequent event is the aggregation of platelets, the release of thromboplastin from the tissues and the appearance of a red thrombus.
The latter is retractable, capable of aseptic lysis, and consists of fibrin, erythrocytes, and platelets.
In the future, the behavior of a thrombus is influenced by the processes of fibrinolysis and coagulation.
The action of fibrinolysin leads to lysis within three to four days, most of the thrombus is destroyed, fragmented, displaced and can move to the pulmonary arteries.
In the future, the formation can resolve without hitting the venous wall or be replaced by connective tissue if the thrombus is of a significant size, and the area of adhesion to the wall is quite long.
With extensive varicose veins, the thrombus settles in the overlying veins or spreads to the perforating veins and deep veins of the affected surface of the lower limb. Deep vein thrombosis involves the spread of a thrombus to the femoral and popliteal veins, while the discharge of blood from them can stop thrombosis in the ascending line.
Clinic of the disease
Symptoms of thrombophlebitis of the deep veins of the lower extremities depend on the location of the thrombus and the degree of its spread and changes in venous patency (obstruction or stenosis of the lumen), the occurrence of collaterals. Clinical manifestations are versatile - from the asymptomatic course of the disease to severe pain and extensive edema, sometimes it ends with gangrene of the extremities.
Asymptomatic flow is typical for the case when the venous outflow occurs without obstacles, while the situation is difficult to recognize and the indicators are characteristic of only one limb.Sometimes the first noticeable sign is only arterial thromboembolism in the lungs. Manifestations of the disease occur transiently - within two to three hours to two days from the appearance of a blood clot:
- ankle, foot, distal leg swell;
- soreness is felt with light pressure on the muscles of the lower leg;
- there are pains in the calf when the foot is bent in the back position and calm down at rest;
- at the site of the lesion, the lower leg becomes hot due to inflammation and increased blood flow;
- dilated superficial veins are observed;
- there is a difference in size around the circumference between the affected and normal limb.